Exercises for Lower Back Pain
A very important part of lower back pain management is exercise prescription. Exercises for lower back pain can be used to improve a variety of potential causes of your back pain. These can include reducing stiffness in the area, improving motor control (activating the correct muscles), improving your strength in the lower back region and associated other areas.
With any back pain, it is ideal to consult your Physiotherapist to have a treatment plan individualised to your injury. If you book in for a session at Barefoot Physiotherapy, your lower back pain treatment plan will typically include; manual therapy, advice and education, stretching or trigger point releases, self-management strategies and exercises to improve your lower back pain. When reducing pain, a part of the treatment plan is helping clients understand how they can prevent their lower back discomfort from reoccurring. It is very important to ensure clients have good work postures, exercise techniques, manual loading, and heavy lifting ergonomics in this instance. When you move well, you are less likely to overload your muscles and injure yourself.

Lower Back Pain Exercise Examples
There are some typical exercises and stretches examples listed below that clients will often be prescribed for their lower back pain management; however, it is recommended your consult your health professional to decide what works best for your body.
- Glute trigger point releases with a lacrosse ball
- Glute stretches
- Hip flexor stretches
- Child’s Pose Stretch
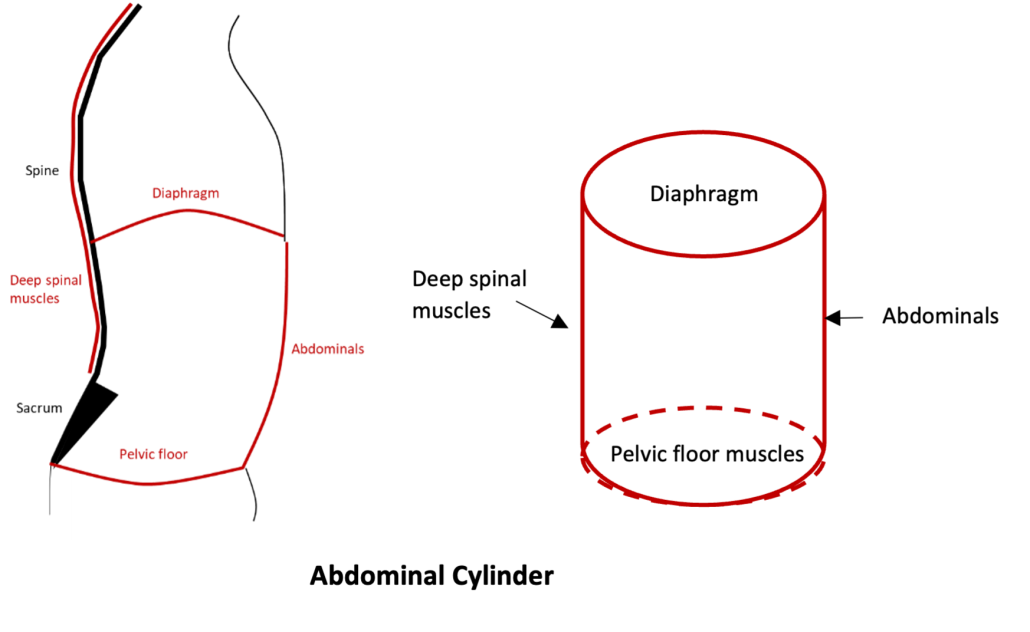
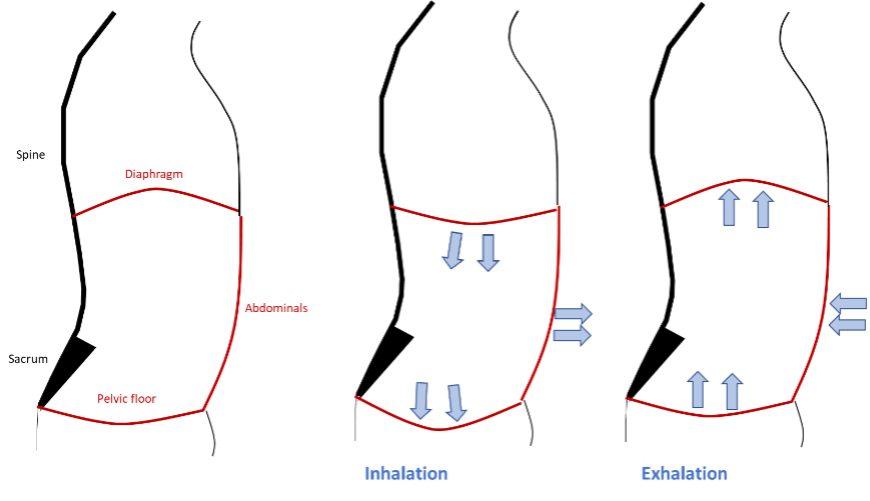
- Deep 360-degree breathing exercises
- Pelvic tilts
- Glute activation squats
- Cat / Cow stretch
- Step ups with glute activation focus
- Weight shift with a focus on glute activation
On our website under the Learn More tab we have a variety of lower back exercises for your reference. Click here to learn more.
If you are experiencing any of the lower back pain symptoms mentioned, please don’t hesitate to reach out to the friendly team of Physiotherapists at Barefoot Physiotherapy. They can help relieve your pain and improve your quality of life. You can give us a call on 1300 842 850 or book online.
W