What is Chronic Pain?
What Is Chronic Pain?
Chronic pain has typically been defined as pain persisting for more than 3 months. This pain can be experienced throughout the entire body, or at localised body parts. Pain is a wonderful tool for our body to protect us from perceived threat of tissue damage. However, so often our ability to accurately determine this threat is altered.
When we experience chronic, or persisting, pain it can have a large impact on all facets of our lives. It may mean that we are unable to participate in social situations, or struggle to maintain strength and mobility. Experiencing chronic pain takes up a portion of your daily energy and brain space, so you may also find yourself being distracted, forgetful or irritable. It’s a multifactorial experience, and requires a multiple factorial approach to treatment.
Considering what is chronic pain and what contributes to chronic pain is a complex process. We know that pain can be increased by not enough sleep, by increased systemic inflammation, by stressful situations and by lack of social/ medical support etc. While initially this may seem overwhelming, it actually means that there are multiple avenues that we can explore to help improve your chronic pain.
The Difference Between Acute and Chronic Pain
This section will compare what is acute pain and chronic pain. The obvious difference between acute and chronic pain is the length of time that pain is experienced. Acute pain usually occurs with a relatively sudden onset and often interferes with mobility and function. It can often be associated with a specific incident, or mechanism of injury, where a particular fall, movement, landing etc. occurs just before the pain begins. This can indicate the presence of tissue damage, or a suddenly provoked protective response from the body. Acute pain has a rapid spike in symptoms for the first few days to weeks, then can decrease steadily over the next few weeks, lasting no longer than 3 months.
Continuing to compare what is acute pain and chronic pain, chronic pain continues to persist long after the initial tissue damage or threat has gone. When considering what is chronic pain, there is often a mismatch in the symptoms felt, and the activities or movements that provoke these symptoms. As mentioned above, nociceptors may be trained to activate at a lower threshold. Hyperalgesia is when something that may usually cause only a minor pain response can be exaggerated (eg a light scratch causing immense pain). Allodynia is when a non-threatening stimulus causes pain (eg a feather lightly touching the skin may feel like a cut). These are just two ways in which the information received from the body can be mis-identified, causing a painful response.
The Causes of Chronic Pain
As mentioned above, pain is a sensation created from contextual information following activation of nociceptors from a perceived threat to body tissues. Chronic pain is the continuation of these painful sensations beyond normal tissue healing timeframes, or in the absence of any tissue damage.
When trying to define chronic pain and what causes it, It is important to appreciate that we don’t have specific “pain receptors” in our body that become activated causing “pain signals”. Instead, we have nociceptors or free nerve endings that respond to changes in mechanical, thermal or chemical stimuli. I.e changes to movement/pressure, temperature or chemicals such as histamine. These nociceptors are activated and send electrical signals up to the brain. It’s in the brain that these signals are interpreted and contextual information is added. If enough nociceptors are activated, and enough “danger” context is added, then the outgoing information that we feel in the body is pain. When we experience what is chronic pain, these nociceptors are being more frequently activated, and/or the danger context is being added much more quickly and frequently regardless of the threat of actual tissue damage.
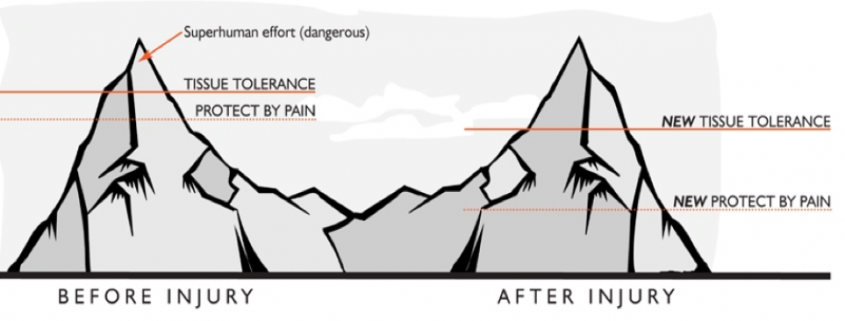
The NOI Group (where so much of the latest research in pain science research and education comes from), describes a dynamic protective buffer between the onset of protection by pain, and the tissue’s actual tolerance before damage begins to occur. This is a warning system the gives us physical signals that we are about to push into our tissue’s threshold.
TWIN PEAKS IMAGE
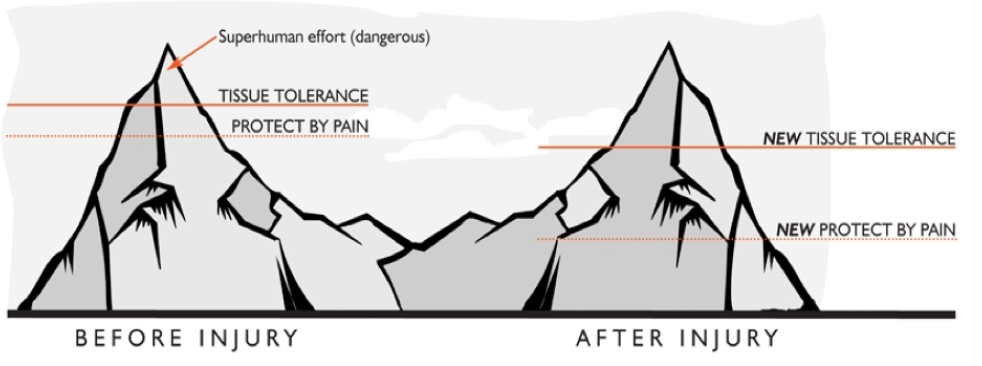
You may push into this buffer slowly, eg running a marathon that you haven’t properly trained for, or quickly, eg a sudden burst of increased physical activity and experience pain and potentially tissue damage. After this tissue damage has occurred, your protective buffer adjusts. Your protect by pain threshold is lowered and you’ll experience the same or similar response as you did before but now at a decreased amount of effort/ load/ activity. This protective buffer can also be influenced by the overall inflammation in the body, stress, expectation of pain, lack of physical conditioning, poor sleep and nutrition or a history of physical injuries.
The Symptoms of Chronic Pain
It can be difficult to define chronic pain beyond the persistence of pain over 3 months. The symptoms that people experience are complex and varied. Chronic pain may be caused by underlying conditions such as endometriosis, arthritis, ankylosing spondylitis or fibromyalgia and chronic fatigue. When we initially think of chronic pain symptoms we immediately think of the physical: dull, achy pain, sharp shooting pain; pins and needles or burning etc. Other chronic pain symptoms include decreased sleep, decreased participation in social interactions or physical activities, increased irritability, decreased concentration, decreased productivity. Unfortunately, the list is long, which is why it’s so important for us to address the whole person in treatment of chronic pain. Similarly, when asked how long is chronic pain, the answer can’t be easily given as it depends on the person, scenario, and interventions.
Understanding the Mental Health Impact of Chronic Pain
The mental health impact of chronic pain is significant. As mentioned above there are so many situations where chronic pain can have a negative impact. Mental health issues and chronic pain go hand in hand. Those experiencing persisting pain are more predisposed to symptoms of depression, anxiety or psychological distress. This relationship works in both directions, people with diagnosed depression or anxiety are more likely to experience chronic pain. The pain itself can be further be influenced by low mood, rumination, inability to sleep and social isolation, often creating an important cycle to break.
How to Manage and Treat Chronic Pain
As chronic pain is a multifactorial experience it means there are so many strategies to help manage your pain. Ultimately we want to change the chronic pain meaning in your body and increase the amount of activity you can do before the protect by pain response is triggered (remembering the protective buffer from before). We do this by finding our ‘Goldilocks’ Zone’; not too little, not too much, but just right! There are many things that help to support this zone. It’s difficult to say how long is chronic pain, as it differs for the individual. Here are some tips that consider the physical, mental and social aspects of chronic pain.
- Increase the amount of incidental activity you do by gradual amounts.
- Pick an activity you can accomplish without causing a flare up (eg a 7 minute walk), repeat that more frequently. General exercise has an overall anti-inflammatory effect on the body.
- Pick a meaningful activity to do more of. You might find that picking up your grandchild is much more comfortable than picking up dirty laundry.
- Change the context! Repeat the activity but in an environment you enjoy. Eg a walk by the river, or to a café with a friend.
- Try to sleep more. Go to bed when you are tired, sleep in a dark and quiet room, avoid caffeine later in the day and avoid screens before bedtime.
- Add in a mindfulness/meditation. Even a brief mindfulness activity can help to balance the nervous system and assist in decreasing inflammation.
- Eat food that makes you feel good! Try to add in one more fruit or vegetable to your meals and vary the colours of your food.
- Aim to focus on your function versus your pain. The more attention we give our pain the more overwhelming it feels.
- Ask for help! Have an engaged team of health professionals to assist you in creating a plan and to support you in this journey. This can include a Physiotherapist, a Psychologist and a GP.
How Barefoot Can Help with Chronic Pain
If you are suffering with chronic pain and don’t know where to start, get in touch. The physiotherapists at Barefoot Physiotherapy can help you create a plan to get you moving and back in control.

 NOI group
NOI group





Leave a Reply
Want to join the discussion?Feel free to contribute!