How Physio Can Help Nerve Irritation
What is Nerve Irritation?
Nervous tissue is designed to be able to smoothly glide in and around the interface of our muscular and skeletal systems. Our bodies are designed to move, therefore our nervous system needs to move with us. When there is nerve irritation, there can be restrictions to our normal freedom of movement. Therefore, physio can help with nerve irritation.
The nervous system underpins all our bodily functions, and one of its primary roles is that of protection – reacting to real or perceived threats that may compromise our safety – think about flight/fight/freeze reactions. It may be caused by stress responses, inflammatory processes, or points of restriction along adjacent tissue structures (e.g. tight muscles, stiff joints or a disc bulge as the nerve travels past or through).
Examples:
- Think about a sprained ankle – our body’s response is to protect it while the tissues are healing: we want to offload the joint, so our body will register pain if we try to overexert ankle movement.
- In today’s world, traditional forms of threat (like wild animals attacking you) are less common, but we still get stress responses to other things that can be physical or less tangible, like that caused by work/home life, relationships, etc. These forms of stress are just as effective as eliciting a protective response by the nervous system.
What Does Nerve Irritation Feel Like?
It can be different for everybody, and may include any one, or combination of:
- Pins and needles
- Numbness
- Sharp pain
- Shooting pain
- Radiating pain
- Tight muscles that don’t seem to release
- Headaches
- Heaviness, or weakness in muscles
Some of the most familiar, traditional examples of nerve irritation include sciatica and carpal tunnel syndrome.

How Can Physio Help With Nerve Irritation?
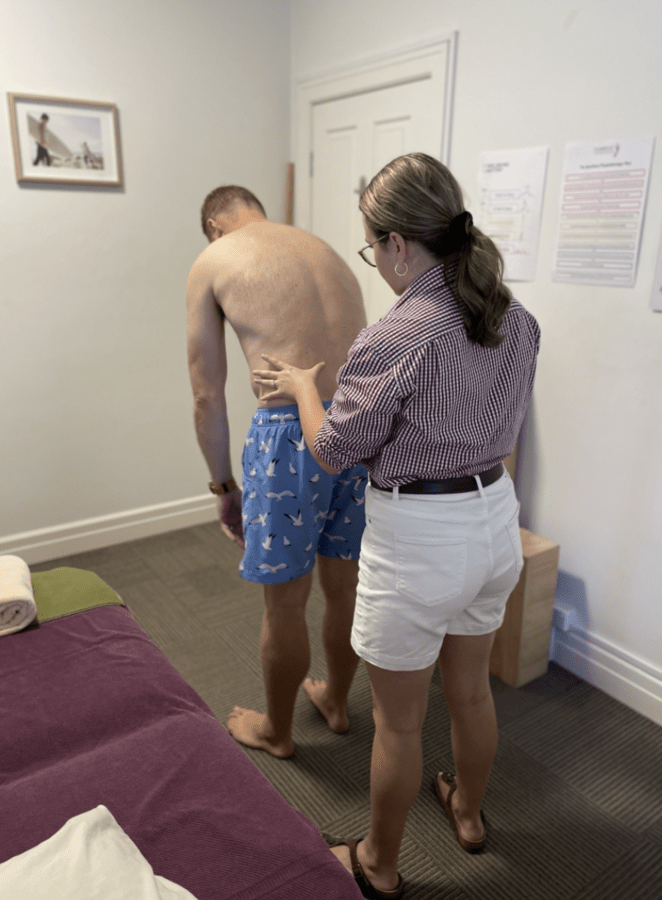
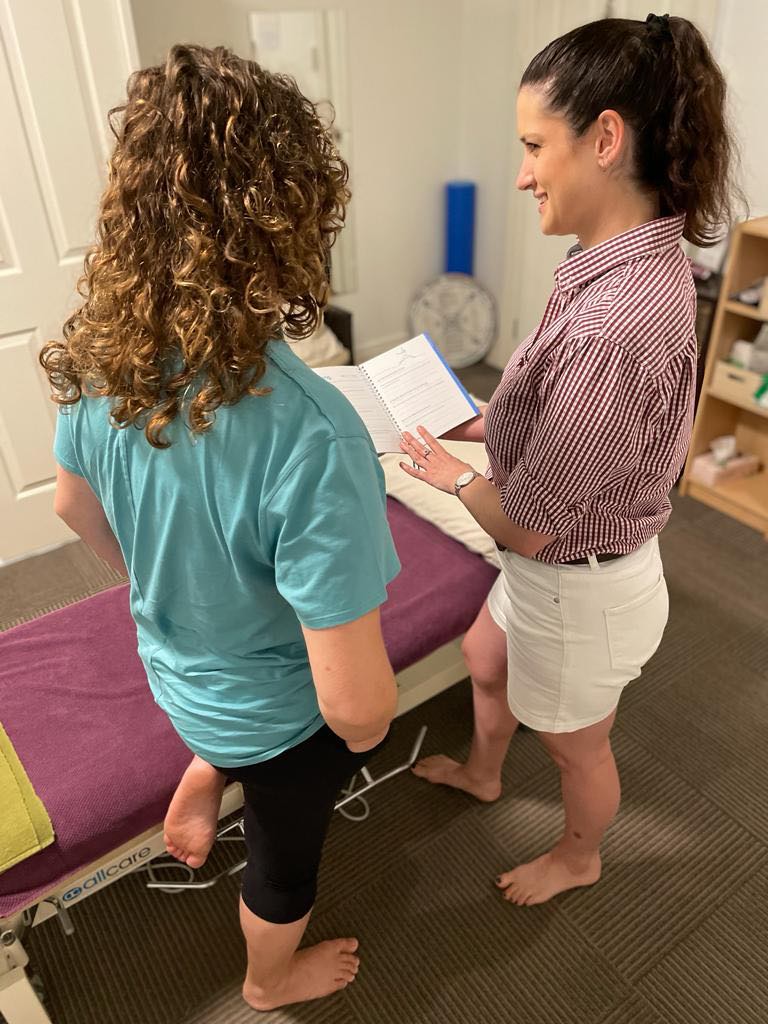
Assessment: gentle neurodynamic (“nerve movement”) tests to assess for nerve irritation. When there is no nerve irritation, our body is comfortable to move through its fullest ranges of movement, with no signs of “guarding” (muscles tightening to restrict this movement)
Following an assessment of spinal joints, your physiotherapist will tease out the most effective joint treatment for your body, where there will be repeated re-assessment to make sure treatment is making the most effective changes.
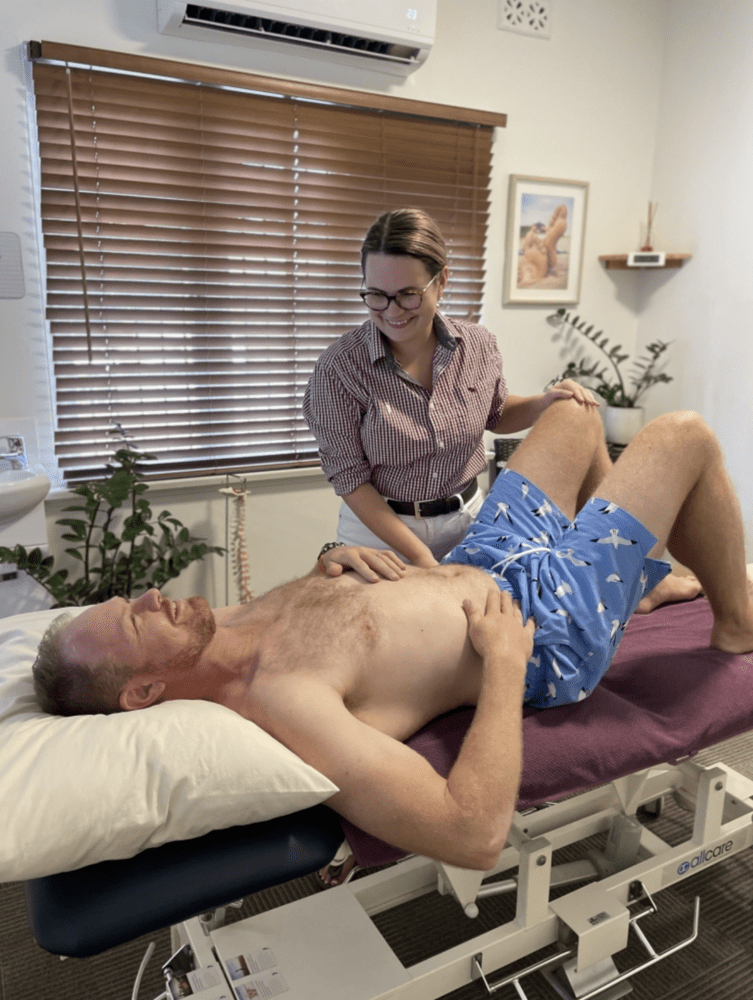
Treatment: may include a number of different modalities to reduce nerve irritation and, then to reduce the likelihood of recurrence. At Barefoot, we will also explore the reasons why there is nerve irritation – is it due to physical loads and postures, stressors, lack of hydration/nutrition, etc.
- Gentle joint mobilisation and muscle releases to reduce points of tightness and restriction in the body
- Motor control – how our body moves and what muscles are contributing to the movement to deload irritated structures and help with movement efficiency
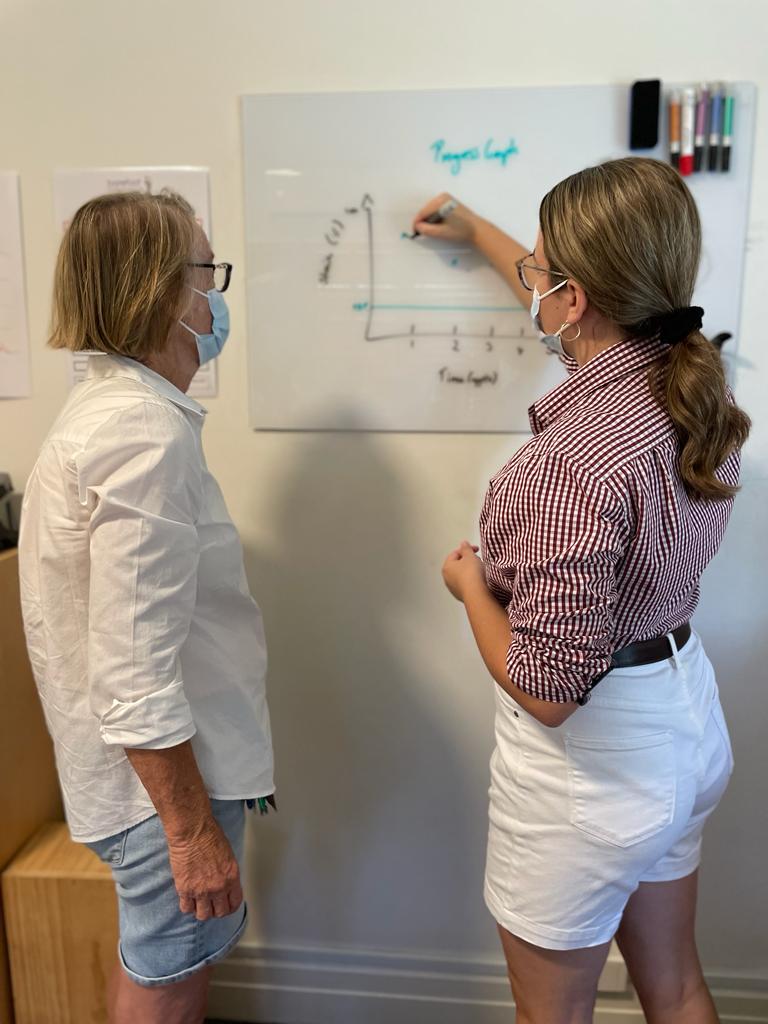
- Postural/ergonomic setup as appropriate for the positions you hold your body – this may include sleep position, sitting position, standing position, or other postures that occur during the most common daily activities you perform
- A collaborative discussion with you regarding other potential related factors such as sleep quality/quantity, nutrition, hydration, emotional loads and stress, etc – see Brain Overload
If you have been experiencing pain, tightness, or other symptoms that may indicate nerve irritation you can click here or phone the clinic on 1300 842 850 to see one of our physiotherapists and get started with a comprehensive nerve assessment and treatment plan. If you enjoyed this blog you should check out our blog on What Is Nerve Pain.