Should I go to Emergency or Physio for my Lower Back Pain?
An acute episode of severe lower back pain can be very debilitating and often people are unsure of where to go to get help. Often people struggle to identify if the type of pain they are experiencing means they should visit the GP, Physio or in some cases the emergency department. Therefore, this blog aims to help you identify through your symptoms the best first step for you. If you are ever unsure please call your local GP or Physio clinic and they can help guide you as well.
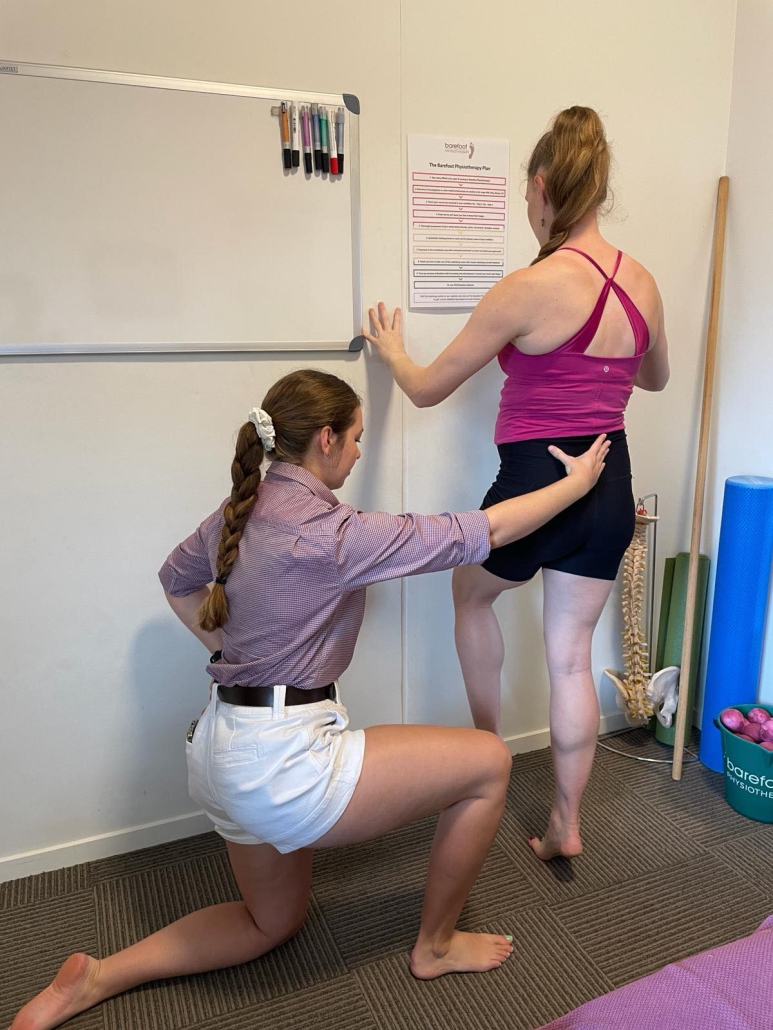
Physiotherapists often see clients who are in very acute episodes of lower back pain, some of these clients have been to emergency or to see their GP before visiting us and some present to us first. As first contact practitioners ie you don’t need a referral to see a Physiotherapist, it is our duty to determine if physio is the right place for you or if we need to refer you on for further medical care. As a general guide I have listed below the signs you should present to Emergency or GP vs the signs Physio would be right for you.
Signs to present to Emergency for Lower Back Pain
- You have severe pain that means you are unable to walk, sit or stand. You physically cannot move due to the pain.
- You have bladder/bowel retention and dysfunction
- Loss of sensation in your pelvic region
- You have sustained a traumatic injury
- There is blood in your urine
- You are experiencing fever / chills and weight loss with your episode of lower back pain
Signs to present to Physiotherapy for Lower Back Pain
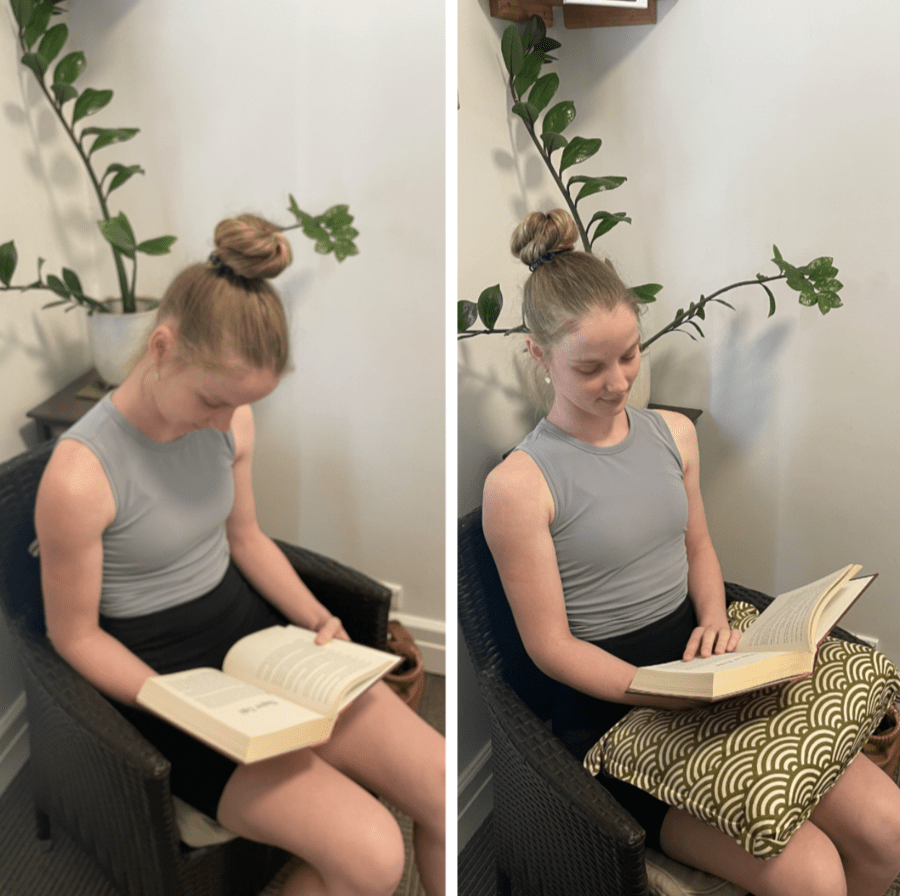
- You have lower back pain that is moderate to severe but are still able to walk/ sit and stand. (may be limited by pain and not for very far distances)
- You have an acute episode of lower back pain after exercise, work or another movement related action.
- You have numbness and tingling or pins and needles in your back and legs but you still have control of your bladder and bowl and have not lost sensation in your pelvic region.
- You have ongoing persistent lower back pain
- You have lower back pain that is sharp, dull or achey
It is important to be alert to any worsening changes in your symptoms and please report those immediately to your Physio or GP.
What are your options?
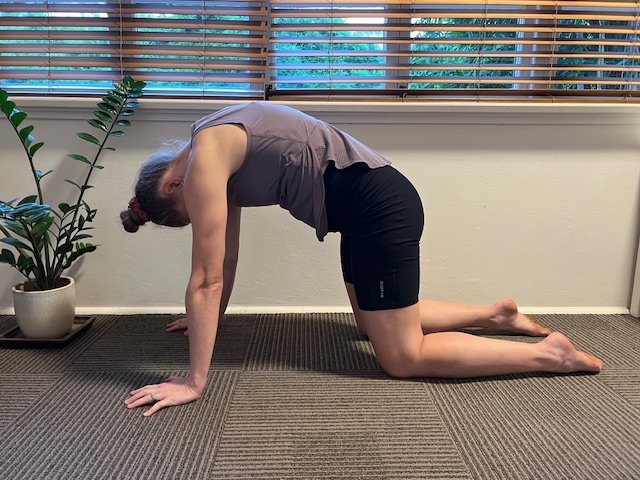
In summary, it is required you present to the Emergency department or immediately to your GP when it is likely your treatment is going to include, significant pain relief through medication, further imaging/tests that require a doctor to carry them out, tests to rule out spinal cord involvement and nerve damage and/or symptoms that may indicate traumatic injury/ surgical intervention required. Therefore, when your treatment isn’t going to require significant medical management it is indicated to present to Physiotherapy. Where your Physiotherapist can provide conservative lower back pain management including manual therapy techniques, mobility exercises, light strengthening and muscle releases/ joint mobilisations and a referral to the GP if necessary.

If you have lower back pain and would like to see a Physiotherapist please click here to book in online. To speak to a Barefoot physio please call us on 1300 842 850. If you found this blog interesting please check out our blog on How Can Physiotherapy help Lower Back Pain.